COVID-19,Pilipinas, tuloy ang laban kontra COVID-19
Pilipinas, tuloy ang laban kontra COVID-19
4/08/2020 10:12:00 PM
Media Center
0 Comments
4/08/2020 10:12:00 PM Media Center 0 Comments
Inanusyo ng Department of Health (DOH) nitong Abril 8, 2020 ang 106 na bagong kaso ng COVID-19 dito sa bansa kaya’t pumalo na ang bilang nito sa 3,870.
Umakyat na rin ang bilang ng mga namatay dahil sa sakit sa 182 ngunit nadagdagan naman ang mga gumaling na ngayon ay 96 na katao na.
Ang unang kaso ng COVID-19 dito sa bansa ay naitala noong Enero ngunit nagsimula ang mabilis na pagdami ng kaso noong Marso. Nagpatupad ng Metro Manila Enhanced Community Quarantine (ECQ) noong Marso 15 at kalauna’y naging Luzon lockdown, na naunang ibinalitang nakatakdang matapos sa Abril 14, 2020. Gayunpaman binanggit ni Cabinet Secretary ng Department of Interior and Local Government (DILG) Karlo Nograles na inaprubahan ni President Duterte ang rekomendasyon ng Inter-Agency Task Force for the Management of Emerging Infectious Diseases (IATF-EID) na ipagpatuloy ang lockdown hanggang Abril 30, 2020.
Marami ang sang-ayon sa naturang ekstensyon. Isa na rito ang pangalawang pangulo na si Vice President Leni Robredo na sinabi sa isang interview sa ANC na “Sang-ayon ako (ipagpatuloy ang lockdown) dahil ‘yong nakikita natin na mga projections, makabubuti para i-flatten ‘yong curve kung hahabaan pa ito, pero tingin ko kasi crucial, crucial para mag-cooperate ‘yong mga tao, crucial na naiintindihan nila kung bakit kailangan ‘tong gawin. Kasi kapag hindi nila naiintidihan kung bakit kailangan ‘tong gawin, ‘yong resistance nandiyan.”
Upang manatiling updated sa mga nangyayari, maaaring magbasa sa mga sites ng news agencies.
May binuo ring grupo ang mga mag-aaral ng UPIS. Maaaring maging updated sa pamamagitan ng pag-follow ng COVID-19 PH Bot sa twitter na pinamamahalaan nina Christian Sarabia, Bree Catibog, Danie Cabrera, Klyssa Betito, at Cresel Lawas mula sa UP Rural High School.
Batay kay Christian Sarabia, nakukuha ang impormasyon ng kanilang COVID-19 PH bot tulad ng bilang ng mga kumpirmadong kaso, PUI, PUM, bilang ng mga namatay at gumaling sa sakit mula sa DOH ncov tracker at pag-check ng iba pang online sources kaugnay ng COVID-19 updates. //ni Mariel Diesta
(COVID-19 PH bot twitter: https://twitter.com/PHCovid19)
(DOH NCOV tracker: https://ncovtracker.doh.gov.ph/)
COVID-19,COVID-19 Campaign: What Can We Give Our Frontliners?
COVID-19 Campaign: What Can We Give Our Frontliners?
4/08/2020 08:25:00 PM
Media Center
0 Comments
4/08/2020 08:25:00 PM Media Center 0 Comments
COVID-19,Opinion: A vital role on the COVID-19 pandemic
Opinion: A vital role on the COVID-19 pandemic
4/08/2020 08:10:00 PM
Media Center
0 Comments
4/08/2020 08:10:00 PM Media Center 0 Comments
On April 7, 2020, the number of confirmed COVID-19 cases in the Philippines reached 3,660, the death toll climbed up to 163, and a total of 73 people have already recovered from the disease.
Given the current supply of testing kits, Jack Ma’s donation of 57,000 COVID-19 testing kits, and the newly approved kits produced by UP, people are pushing for mass testing that prioritizes Persona Under Investigation (PUIs), Persons Under Monitoring (PUMs), and frontliners, such as healthcare personnel, security guards, custodial workers, and military forces.
According to COVID-19 response head Carlito Galvez, Jr., the government is eyeing to conduct mass testing beginning April 14. However, he clarified to the media that testing is ongoing and the Department of Health (DOH) has already tested 22,958 people as of April 6, 2020. The importance of testing has been frequently emphasized by the World Health Organization and by countries with best practices for curbing the spread of the virus for it will help to see the real numbers and even detect those who have the disease but are asymptomatic. Without mass testing, this lockdown will be useless.
However, with the number of COVID-19 patient cases, and PUIs and PUMs continuously rising, some medical centers are running out of space to accommodate new patients. Hospitals such as Makati Medical Center, The Medical City in Pasig, St. Luke’s Medical Center in Quezon City and Bonifacio Global City, Chinese General Hospital, The Asian Hospital and Medical Center in Muntinlupa, and Delos Santos Medical Center in Quezon City, have released separate announcements that they are already at capacity. Since it is highly possible that the number of cases will increase with amped up testing, the government has to be prepared and should have an effective system in place.
Last April 3, Presidential Adviser for Flagship Programs and Projects Vince Dizon told the media that the National Government Administrative Center in New Clark City in Capas, Tarlac will become a temporary hospital which can house about 1000 patients. The Athlete’s Village will also be used as a quarantine facility. On the same day, the government started converting the Philippine International Convention Center (PICC), World Trade Center, and the Rizal Memorial Complex into COVID-19 isolation centers. The government, together with the LGUs, needs to act urgently and efficiently in converting facilities into COVID-19 isolation centers to prepare for the COVID-19 peak.
Unfortunately, rooms for COVID positive patients aren’t the only problem of hospitals. They are also running out of supplies of Proper Protective Equipment (PPE) and have started asking for donations. Since healthcare workers are most exposed, it is a must that they be provided with enough PPE so that their work is unhampered. Part of the 275B-peso budget allocation as stated in Republic Act No. 11469 or Bayanihan to Heal as One Act would be used to provide PPEs for our frontliners.
In another late-night address on April 6, President Duterte mentioned that all resources in the Bayanihan Act have already been allocated. This covers funding for the Department of the Interior and Local Government (DILG) to assist the LGUs in providing aid for their people, particularly to poor families. People who are earning minimum wage, no work no pay, street vendors, and those whose source of family income is driving public vehicles, should be prioritized by the government for they are the people who can’t stock-up basic necessities, which make them vulnerable to starvation. This will tide them over until the end of the extended ECQ on April 30.
These programs and guidelines will be more effective if everyone would do their part as individuals.
Citizens can also help by staying at home, as much as possible, unless it's necessary to go out to buy food and medicine. Always disinfect by washing your hands with soap for not less than 20 seconds. With cooperation, smooth communication, and proper prioritization and allocation of resources, more lives may be saved. //by Mariel Diesta
COVID-19,COVID-19 Campaign: What is the Philippines Doing in Response to COVID-19?
COVID-19 Campaign: What is the Philippines Doing in Response to COVID-19?
4/08/2020 08:05:00 PM
Media Center
0 Comments
4/08/2020 08:05:00 PM Media Center 0 Comments
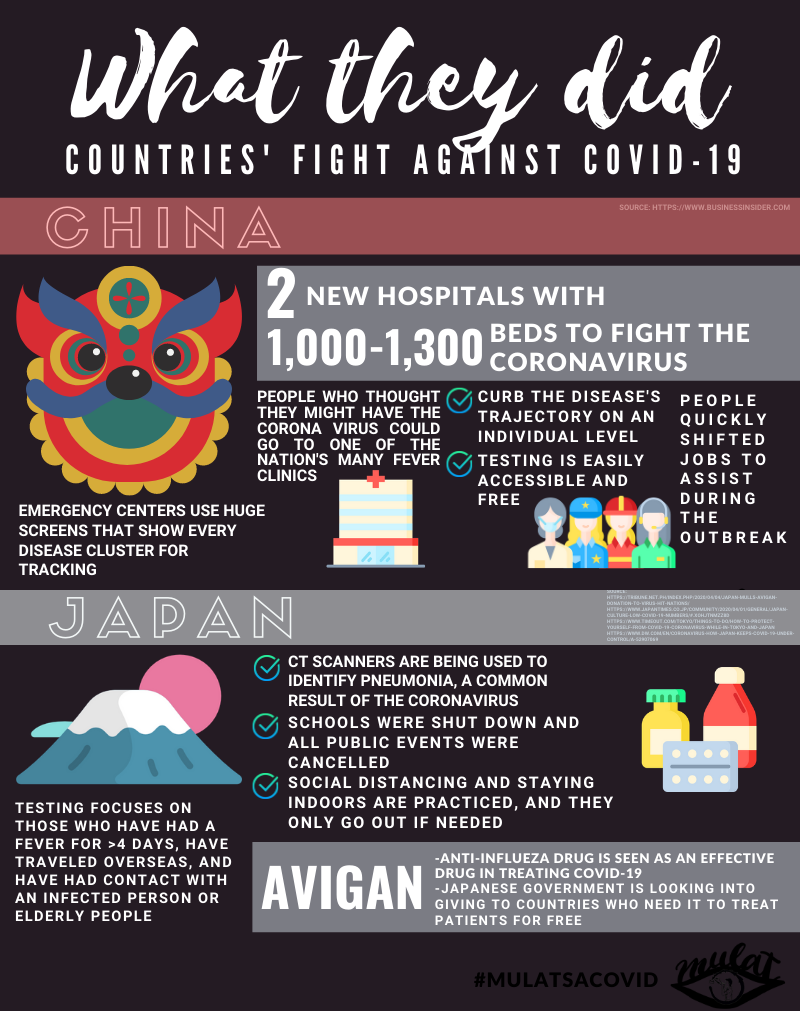
COVID-19,COVID-19 Campaign: Countries' Fight against COVID-19
COVID-19 Campaign: Countries' Fight against COVID-19
4/08/2020 08:00:00 PM
Media Center
0 Comments
4/08/2020 08:00:00 PM Media Center 0 Comments
angelia albao,Health & Sciences: A consolidated scientific guide in understanding COVID-19 (Part 2)
Health & Sciences: A consolidated scientific guide in understanding COVID-19 (Part 2)
4/08/2020 07:45:00 PM
Media Center
0 Comments
4/08/2020 07:45:00 PM Media Center 0 Comments
As mentioned in the first part (http://upismc.blogspot.com/2020/04/health-sciences-consolidated-scientific.html) of our coronavirus disease (COVID-19) guide, the disease, which spreads quickly, now greatly affects our lives. For the second part of the guide, scientific progress in the battle against COVID-19 will be discussed. Science-proven ways on how the further spread of the virus could be prevented will also be recommended.
Scientific developments done to fight COVID-19
Scientists have tried to invent quick, efficient diagnostic testing methods for COVID-19. These testing procedures use reverse transcriptase polymerase chain reaction (RT-PCR) (Lanese, 2020; Magsambol, 2020). In this mechanism, a swab is applied to someone’s throat. It detects and collects viral ribonucleic acid (RNA), one’s basic genetic material.
Afterwards, the RNA primers having a particular nuclear acid sequence bind with primase; thus, facilitating the reverse transcription from RNA to complementary deoxyribonucleic acid (cDNA). Remember that the central dogma of molecular biology lets DNA become messenger RNA (mRNA) in transcription. In RT-PCR, the other way around happens – RNA becomes cDNA; hence, being “reverse”. Then replication of the transcribed DNA occurs with a processing machine. Once there are ample samples, the genetic material bits are exposed to UV light via fluorescence. If they glow, then SARS-Cov-2 is present in the patient’s blood (Lanese, 2020; Merck, 2020).
Figure 1. The RT-PCR visualized in a diagram.
While RT-PCR is known to be “highly specific”, there is a 30% probability that the results may be false (Lanese, 2020). This usually happens when samples taken from patients are incomplete. This kind of test kit is what the Philippine government has received from other countries ever since the proliferation of cases in the country (ANC, 2020). While there have been donations from the World Health Organization (WHO), other test kits have been imported with a rate of PHP 8,000 per unit.
The quality, expenses, and time elapsed from receiving help from other countries prompted our scientists in the local level to create their own test kits. In fact, microbiology and biotechnology expert Dr. Raul Destura and the scientists from the University of the Philippines (UP) have developed a low-cost COVID-19 testing kit: the GenAmplify™ Corona Virus 2019 (COVID-19) Kit.
This detection kit is different from the RT-PCR kits in a sense that it uses a single step multiple detection system. This system has a turnaround time of just one to two hours, contrary to other COVID-19 detection kits' 6-hour turnaround time. The COVID-19 test involves getting samples from inside the patient’s nose and from the back of their throat with a brush for the nasopharynx, the upper part of the pharynx, and swab similar to that being used in RT-PCR (ANC, 2020).
Aside from this, Dr. Destura adds that there are three vials, “The first is a reagent used to extract the genetic material from the sample. The other is an amber-colored chemical that makes the virus fluorescent for detection. And the third vial is molecular-grade water that serves as negative control to ensure that the results are accurate” (Sabillo, 2020).
Figure 2. The RT-PCR test kits developed by our local scientists. Notice the three vials beside the kit box. Source: https://newsinfo.inquirer.net/1253582/fda-approves-up-developed-covid-19-test-kits-for-commercial-use
The test kits had already passed the field validation phase and were awarded a Certificate of Product Registration by the Food and Drug Administration (FDA) last April 3 (Yumol, 2020). The test kits can be used for up to 120,000 tests. In addition, 1,300 of the test kits will be distributed to the following hospitals (Magsambol, 2020):
• Philippine General Hospital, Manila,
• Makati Medical Center,
• The Medical City, Pasig City,
• Baguio General Hospital,
• Vicente Sotto Memorial Medical Center, Cebu City, and
• Southern Philippines Medical Center, Davao City
The remaining test kits will then be sold by Manila HealthTek at around PHP 1,300 per kit, much cheaper than other test kits that are currently being sold at around PHP 8,000 per kit (ANC, 2020).
Meanwhile, there have been concerns about the formulation of a drug and a vaccine for COVID-19. As of now, there are no official antiviral drugs and vaccines for the disease (Rothan & Byrareddy, 2020; WHO, 2020). For the former, chloroquine (against malaria), arbidol (against influenza), remdesivir (against ebola), and favipiravir (against influenza, West Nile virus, etc.) are being tested in terms of their effectivity and safety (Dong, Hu, & Gao, 2020). Meanwhile, it will take a year and a half to manufacture the latter for public use (Grenfell & Drew, 2020).
Ways we could prevent contracting and spreading COVID-19
Now that we know what our scientists have invented, let’s focus on how we could help as concerned citizens in avoiding the contraction and transmission of the virus.
1. Stay at home.
Staying at home is an effective way to slow down the spread of the virus. Remember, people with the disease can be asymptomatic, so even if the people around us don’t have a cough or fever, they can still be carriers of the disease (WHO, 2020; Woodward, 2020). Once we go outside, we come across multiple people, not knowing if they’re infected or not. To avoid risking ourselves getting the virus, it is better to stay home.
Additionally, staying at home also means that we are eliminating the risk of infecting other people as well. Whether one has symptoms or not, it may be possible that they have the virus, so it is better to stay put in order to not infect other people (WHO, 2020).
2. Maintain social distancing.
Even though it is ultimately best to stay at home, the fact is that some people still have to go outside either to go to work (such as health workers, employees of essential services, etc.) or to buy food. So if ever we are outside, it is best that we maintain social distancing (DOH, 2020; WHO, 2020).
What is social distancing? Social distancing is a health practice done to lessen the chances of a sick person transmitting a contagious disease to a healthy person. It is done by maintaining at least 6-feet (or about 2 meters) distance between us and the people around (Letzer, 2020).
Why should we practice social distancing? When people sneeze or cough, they spray out droplets in the air, which can then be inhaled by the people near them (WHO, 2020; Woodward, 2020). If an infected person sneezes or coughs, the droplets they emit will have the virus, which can then be passed on to those who inhale the droplets (Rothan & Byrareddy, 2020). Six feet is the average distance that the droplets from coughing/sneezing travel in the air before they settle. By maintaining at least a 6-feet distance between us and the people around, both sides eliminate the chances of acquiring or transmitting the virus via the droplets (Letzer, 2020).
Even when we’re at home, it is still important to keep a safe distance. If it is possible to keep a 6-feet distance between us and the people in our home, then we should do so. But if it is not, we should try to limit our contact with them at least and to maintain as much distance as wecan, especially if there is a person who is vulnerable to COVID-19 in our home (WHO, 2020).
3. Wash hands and clean things
Our hands often can acquire germs and viruses – not to mention, the very coronavirus, from the many surfaces that we touch throughout the day. Thankfully, soap can destroy viruses (Marshall, 2020). Not just antibacterial soap, but even any soap in general.
Soap is made up of molecules that have two parts, a lipophilic end and a hydrophilic end. The lipophilic end, which is attracted to fat, breaks down the coating of fat that surrounds the virus, and literally breaks the virus apart (Thordarson, 2020). So to make sure our hands are clean, we need to wash our hands with soap and running water for at least 20 seconds. If it is not possible, we can use a rubbing alcohol or a hand sanitizer that has at least 60% alcohol content (Marshall, 2020).
When should we clean our hands? According to the Centers for Disease Control and Prevention (CDC, 2020a), we should wash our hands after the following:
• before touching our eyes, nose, or mouth,
• before, during, and after preparing and eating food,
• before and after caring for someone who is sick with vomiting or diarrhea,
• before and after treating a cut or wound,
• after using the toilet/restroom,
• after changing diapers or cleaning up a child who has used the toilet,
• after blowing out the nose, coughing, or sneezing,
• after touching an animal/pet, their feed, or their waste,
• after handling garbage,
• after we have been in a public place, and
• after we’ve touched an item or surface that may be frequently touched by other people, such as door handles, tables, gas pumps, shopping carts, or electronic cashier registers/screens, etc.
Aside from washing our hands, it is also important to keep the surfaces and objects around us clean, especially the ones which we frequently touch (CDC, 2020b; WHO, 2020). Some examples of these are our gadgets, our door knobs, and even our tables. To clean these surfaces, we can use soap and water or wipes and alcohol.
4. Boost the immune system
Increasing our immune system is really important in times like this. To give our immune system a boost, it is advisable to have a healthy, balanced meal (DOH, 2020). However, considering the limited resources, if this is not possible, taking essential vitamin supplements such as Vitamin C and Zinc tablets can be done instead as zinc is said to be “proven to protect the throat” (GMA News, 2020).
Aside from this, it is important to stay hydrated and well-rested. We should make sure that we drink at least 8 glasses of water a day and to sleep at least 8 hours a day (DOH, 2020). The right amount of exercise also helps in maintaining our body’s health.
5. Stay updated and informed
As mentioned in the first part of the guide, there are a lot of uncertainties about COVID-19. Since we don’t know much about the virus yet scientists are constantly conducting research to know more about the nature of and how to combat the virus.
To be well-informed on the new advancements about the virus, we should make it a habit to tune in to the news and to research about it on the internet (Brenneman, 2020). Let us make sure that the news we read are from credible sources though, to avoid being misinformed. Before we believe and forward news we receive from our friends or family members (eg. via group chats), we should check the source and assess if it is reliable. Reporting bots and accounts that promote bogus information will also help (Ko, 2020).
We should also cross-check the facts stated in the news we read to verify if the pieces of information stated are valid or not. This is essential in “judging the plausibility of claims”; in other words, seeing if content is believable or not (Brenneman, 2020). If the source is not valid and the facts are not verified by other reliable sources, it is best not to forward the news to other people to prevent the spread of fake news.
As we fact-check, we can regularly check the websites of official scientific organizations such as the Department of Health (DOH), World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC). We can also follow the official accounts of our national and local government to be updated with the latest regulations and policies to be implemented in our area.
Figure 3. DOH infographic for COVID-19 nature, symptoms, and prevention.
Source: http://www.doh.gov.ph/node/19122
To conclude our guide, we would like to share the experiences of Francis Mey, a nurse from St. Luke’s Medical Center in Bonifacio Global City (BGC). As she recovers from COVID-19, she commends the bravery of nurses, doctors, scientists and other workers serving as frontliners. She also urges the public to stop discrimination against the frontliners just because they could be infected by COVID-19 and other diseases, “Sana ‘wag n’yo po kaming pandirian, w’ag n’yo po kaming layuan” [Please do not be disgusted, please do not stay away from us.] (ABS CBN News, 2020).
With that, let us not forget to contribute in the battle against COVID-19 through our small ways. Let us also not forget to appreciate our frontliners. Namely, our leaders implementing safety measures, our doctors treating those infected, and most of all, our scientists deciphering the mystery behind this novel disease.
Sources (in APA format)
• ABS CBN News. (2020, April 3). Nurse na nagka-COVID-19 ibinahagi ang karanasan habang naka-quarantine. Retrieved 4 April 2020 from https://news.abs-cbn.com/video/news/04/03/20/nurse-na-nagka-covid-19-ibinahagi-ang-karanasan-habang-naka-quarantine.
• ANC. (2020, April 3). The low-cost COVID-19 testing kit made by UP scientists is ready for rollout. ABS CBN News. Retrieved 5 April 2020 from
• Brenneman, R. (2020, April 2). To counter COVID-19 misinformation, USC expert backs new approach to science learning. USC News. Retrieved 5 April 2020 from https://news.usc.edu/167626/covid-19-misinformation-plausibility-judgments-science-learning/.
• Centers for Disease Control and Prevention [CDC]. (2020a, April 2). When and how to wash your hands. Retrieved 3 April 2020 from https://www.cdc.gov/handwashing/when-how-handwashing.html.
• CDC. (2020b, April 2). Cleaning and disinfecting your home. Retrieved 3 April 2020 from https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/disinfecting-your-home.html.
• Department of Health [DOH]. (2020). HEALTH ADVISORY TUNGKOL SA CORONAVIRUS. Retrieved 2 April 2020 from http://www.doh.gov.ph/node/19122.
• Dong, L., Hu, S., & Gao, J. (2020). Discovering drugs to treat coronavirus disease 2019 (COVID-19) [Abstract]. Drug Discov Ther, 14(1): 58 – 60. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/32147628.
• GMA News. (2020, January 30). DOH urges the public to wash hands, drink water, eat healthy, avoid crowded places. Retrieved 5 April 2020 from https://www.gmanetwork.com/news/lifestyle/familyandrelationships/724185/doh-urges-the-public-to-wash-hands-drink-water-eat-healthy-avoid-crowded-places/story/.
• Grenfell, R. & Drew, T. (2020, February 17). Here's why it's taking so long to develop a vaccine for the new coronavirus. Science Alert. Retrieved 5 April 2020 from https://www.sciencealert.com/who-says-a-coronavirus-vaccine-is-18-months-away.
• Ko, R. (2020, April 2). Social media Is full of bots spreading COVID-19 anxiety. Don't fall for it. Science Alert. Retrieved 5 April 2020 from https://www.sciencealert.com/bots-are-causing-anxiety-by-spreading-coronavirus-misinformation.
• Lanese, N. (2020, April 3). Even if you test negative for COVID-19, assume you have it, experts say. Live Science. Retrieved 5 April 2020 from https://www.livescience.com/covid19-coronavirus-tests-false-negatives.html.
• Letzer, R. (2020, March 31). Is 6 feet enough space for social distancing?. Science Tech. Retrieved 3 April 2020 from https://www.livescience.com/coronavirus-six-feet-enough-social-distancing.html.
• Magsambol, B. (2020, April 3). U.P.-developed coronavirus test kits ready for mass use beginning April 4. Rappler. Retrieved 5 April 2020 from https://www.rappler.com/nation/256929-up-developed-coronavirus-testing-kits-ready-mass-use-starting-april-4-2020.
• Marshall, M. (2020, March 18). How soap kills the corona virus. Vox. Retrieved 2 April 2020 from https://www.vox.com/2020/3/18/21185262/how-soap-kills-the-coronavirus.
• Merck. (2020). RT-PCR — Reverse transcription PCR. Retrieved 5 April 2020 from https://www.sigmaaldrich.com/life-science/molecular-biology/pcr/rt-pcr.html.
• Rothan, H.A. & Byrareddy, S.N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. Retrieved from https://www.sciencedirect.com/science/article/pii/S0896841120300469?via%3Dihub.
• Sabillo, K. (2020, April 1). Explainer: What’s the difference between PCR-based and rapid test kits for COVID-19?. ABS CBN News. Retrieved 5 April 2020 from https://news.abs-cbn.com/news/04/01/20/different-kinds-of-coronavirus-test-kits-used-in-the-philippines.
• Thordarson, P. (2020, March 12). The science of soap – here’s how it kills the coronavirus. Guardian. Retrieved 2 April 2020 from https://www.theguardian.com/commentisfree/2020/mar/12/science-soap-kills-coronavirus-alcohol-based-disinfectants.
• World Health Organization [WHO]. (2020, February 28). Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Retrieved 4 April 2020 from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
• WHO. (2020, March 18). Basic protective measures against coronavirus. Retrieved 2 April 2020 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
• Woodward, A. (2020, April 3). It's estimated 1 in 4 coronavirus carriers could be asymptomatic. Here's what we know. Science Daily. Retrieved 4 April 2020 from https://www.sciencealert.com/here-s-what-we-know-so-far-about-those-who-can-pass-corona-without-symptoms.
• Yumol, D. (2020, April 3). FDA approves first locally-made COVID-19 test kits. CNN News. Retrieved 5 April 2020 from https://www.cnnphilippines.com/news/2020/4/3/fda-approves-first-locally-made-test-kits.html.
//by Angie Albao and James Tolosa
angelia albao,Health & Sciences: A consolidated scientific guide in understanding COVID-19 (Part 1)
Health & Sciences: A consolidated scientific guide in understanding COVID-19 (Part 1)
4/08/2020 07:30:00 PM
Media Center
0 Comments
4/08/2020 07:30:00 PM Media Center 0 Comments
Lately, the coronavirus disease 2019 (COVID-19) has been hitting cities all over the world. From its discovery in a wet market in Wuhan, the capital of Hubei, China on December 31, 2019 to its widespread transmission to other continents, there have been more than a million cases worldwide (Gutiérrez, 2020). Because of this, the World Health Organization (WHO) declared COVID-19 as a “pandemic” on March 11 because it has spread worldwide and could possibly infect almost everyone (Ducharme, 2020).
Figure 1. Exponential increase of COVID-19 cases across the globe as of April 7. Note that the last point of the graph reached beyond the 1 million x-axis.
Consequently, our governments struggle to deal with the disruption of major industries and sectors. Together with frontliners like nurses and doctors, they cater to the safety and security of our fellowmen. In addition, as we try to understand this new, complex disease, we feel anxious about its possible threats.
Fortunately, scientists are able to relieve our uncertainty. As they debunk bogus rumors about the disease, they give us authentic, credible information. They provide us a more rational and knowledgeable perspective as they undergo intensive research and experiments. For instance, they inform us of the nature of the disease, its effects to us humans, and the ways we could prevent contraction and transmission.
With that, scientific findings for COVID-19 will be summarized in the next paragraphs. In the first part of this guide, the technical aspects of the disease will be discussed.
Epidemiological nature of the COVID-19
WHO (2020) declares that as of February 11, coronavirus disease (COVID-19) is the official name of the sickness itself. Its pathogen is a virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which superseded the name novel coronavirus (2019-nCoV) last January 31.
As suggested by the name of the virus, it belongs to the coronavirus family. According to the Center for Disease Control and Prevention (CDC, 2020), coronaviruses are named for their “crown-like spikes on their surface”. They mainly affect our respiratory system – the system responsible for our breathing (NIAID, 2020). Some coronaviruses that caused similar outbreaks in the past decades include SARS-CoV (which caused severe acute respiratory syndrome in 2002) and MERS-CoV (which caused Middle East Respiratory Syndrome in 2012).
The recent report from the WHO (2020) China Joint Mission classifies COVID-19 as a zoonotic disease. This means that the disease is mainly transmitted through contact with animals. This was firstly assumed as those who frequented the Wuhan wet markets selling livestock and exotic animals contracted the disease. While there’s no determined host as of now, scientists suspect that bats are the reservoirs carrying the SARS-CoV-2 (Bangkok Post, 2020; Rothan & Byrareddy, 2020).
Modes of transmission (MoTs) of the COVID-19
COVID 19 has two MoTs. According to the same report by WHO (2020), the first transmission mainly occurs through respiratory aerosols that are 5 to 10 micrometers wide (Note: This is different from airborne transmission, where the droplets have a diameter of less than 5 micrometers.). These droplets are released when a person sneezes or coughs. They can then be inhaled by people who are nearby. However, since COVID-19 can be spread by people who are asymptomatic (i.e. do not manifest symptoms), even close contact with a person who has COVID-19 is enough to spread the virus (WHO, 2020; Woodward, 2020).
Much scarier, Dr. Harvey Fineberg, chair of National Academy Sciences’ Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats, shares research findings claiming that the virus can be spread through droplets from talking and even breathing. According to him, “...[coronavirus] could be spread via aerosols generated directly by patients' exhalation.” (Guardian, 2020).
The second mode of transmission occurs through fomites. These are objects whose surfaces could be contaminated by the virus. Fomites can be passed onto people if they touch these objects (WHO, 2020). Studies from University of California, Los Angeles (UCLA) and the New England Journal of Medicine suggest that the virus can stay up to four hours on copper, a day on cardboard and even up to 2 or 3 days on plastic and stainless steel (UCLA, 2020; Van Doremalen et al., 2020).
Factors affecting the contraction and transmission of COVID-19
According to Tom Kotsimbos, a respiratory physician, “Anybody can contract COVID-19” (Guardian, 2020). Those 18 years old and below seem to be the least affected group (WHO, 2020). Meanwhile the following categories are at a higher risk for COVID-19:
1. the elderly, i.e. people aged 60 and above (CDC, 2020, Rothan & Byrareddy, 2020; WHO, 2020),
2. those having underlying diseases like asthma (CDC, 2020), hypertension (WHO, 2020; Rothan & Byrareddy, 2020), diabetes (CDC, 2020; Rothan & Byrareddy, 2020), etc.,
3. medical workers and other health care providers (CDC, 2020; Rothan & Byrareddy; WHO, 2020), and,
4. pregnant people, in the sense that they are more susceptible to respiratory diseases (CDC, 2020; Rothan & Byrareddy, 2020)
On the other hand, the factors affecting transmission of COVID-19 are highly variable and thus still unclear (Antrim, 2020; WHO, 2020). Some researchers hypothesize that SARS-CoV-2 could stay in the water or air. Its humidity and temperature could possibly speed up or impede the transmission process itself.
Harmful effects of COVID-19 to the human body
Figure 2. Body system disorders caused by COVID-19.
As mentioned in the introduction, COVID-19 mainly impairs the respiratory system. Its effects are similar to those of MERS and SARS. According to the Department of Health (2020) and Kandola (2020), the SARS-CoV-2 mainly infects the lining of the pharynx (throat), trachea (windpipe), and lungs.
Symptoms vary from person to person. Usually, it takes about 5 to 6 days after infection for a person to display symptoms (WHO, 2020). Common symptoms (reported by around 4 out of 5 patients) include the following (DOH, 2020; WHO, 2020):
1. fever (38º C),
2. runny nose,
3. sweats & chills,
4. coughs and colds, and
5. shortness of breath.
Sources (in APA format)
• Antrim, A. (2020, March 20). Environmental engineers identify factors affecting COVID-19 transmission. Contemporary Clinic. Retrieved 5 April 2020 from https://contemporaryclinic.pharmacytimes.com/news-views/environmental-engineers-identify-factors-affecting-covid-19-transmission
• Bangkok Post. (2020, January 23). Why wild animals are a key ingredient in China's coronavirus outbreak. Retrieved 4 April 2020 from https://www.bangkokpost.com/world/1842104/why-wild-animals-are-a-key-ingredient-in-chinas-coronavirus-outbreak.
• Centers for Disease Control and Prevention [CDC]. (2020, February 15). Human coronavirus types. Retrieved 2 April 2020 from https://www.cdc.gov/coronavirus/types.html.
• CDC. (2020, April 2). People who are at higher risk for severe illness. Retrieved 5 April 2020 from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html.
• Ducharme, J. (2020, March 11). World Health Organization declares COVID-19 a 'pandemic.' Here's what that means. Time. Retrieved 3 April 2020 from https://time.com/5791661/who-coronavirus-pandemic-declaration/.
• Guardian. (2020, March 18). Coronavirus: the science of how Covid-19 affects the human body. Retrieved 4 April 2020 from https://www.theguardian.com/australia-news/audio/2020/mar/19/coronavirus-the-science-of-how-covid-19-effects-the-human-body?fbclid=IwAR1wZET59EdV0CN0VXjgAVEcIlIodqmk7uO67pfRVS3rIyVRJ0ap_2bW1V4.
• Gutiérrez, P. (2020, April 4). Coronavirus world map: which countries have the most cases and deaths?. Guardian. Retrieved 5 April 2020 from https://www.theguardian.com/world/2020/apr/04/coronavirus-world-map-which-countries-have-the-most-cases-and-deaths.
• Kandola, A. (2020, March 25). How does coronavirus affect the body?. Medical News Today. Retrieved 3 April 2020 from https://www.medicalnewstoday.com/articles/coronavirus-effects-on-body?fbclid=IwAR1CXuLBkO2IyBLksdAj-bSeiq3Ls_DOmCme_QdIidKPz5YU9CqPF1GvlzM.
• McKeever, A. (2020, February 18). Here’s what coronavirus does to the body. National Geographic. Retrieved 3 April 2020 from https://www.nationalgeographic.com/science/2020/02/here-is-what-coronavirus-does-to-the-body/?fbclid=IwAR1cpKImt_PqizPjhGARR2vD4yV3mOjNEsU7QtosFXSWTqGZo0Re_j6rz4g.
• National Institute of Allergy and Infectious Diseases [NAIAD]. (2020, March 25). Coronaviruses. Retrieved 4 April 2020 from https://www.niaid.nih.gov/diseases-conditions/coronaviruses.
• Rothan, H.A. & Byrareddy, S.N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. Retrieved from https://www.sciencedirect.com/science/article/pii/S0896841120300469?via%3Dihub.
• University of California - Los Angeles [UCLA]. (2020, March 20). Study reveals how long COVID-19 remains infectious on cardboard, metal and plastic: People may acquire coronavirus through air and by touching contaminated surfaces. ScienceDaily. Retrieved April 4, 2020 from www.sciencedaily.com/releases/2020/03/200320192755.htm.
• Van Doremalen et al. (2020, March 17). Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. Retrieved 4 April 2020 from https://www.sciencedirect.com/science/article/pii/S0896841120300469?via%3Dihub.
• World Health Organization [WHO]. (2020, February 28). Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Retrieved 4 April 2020 from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
• WHO. (2020, March 18). Basic protective measures against coronavirus. Retrieved 2 April 2020 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
• WHO. (2020, March 29). Vías de transmisión del virus de la COVID-19: repercusiones para las recomendaciones relativas a las precauciones en materia de prevención y control de las infecciones [Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations]. Retrieved 3 April 2020 from https://www.who.int/es/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations.
• Woodward, A. (2020, April 3). It's estimated 1 in 4 coronavirus carriers could be asymptomatic. Here's what we know. Science Daily. Retrieved 4 April 2020 from https://www.sciencealert.com/here-s-what-we-know-so-far-about-those-who-can-pass-corona-without-symptoms.
However, in extreme cases, further health complications are possible, such as (WHO, 2020):
1. acute respiratory distress syndrome (ARDS), which causes fluid to leak into the lungs,
2. pneumonia, which inflames the alveoli (air sacs in the lungs) through pus, and
3. multiple organ failure.
1. acute respiratory distress syndrome (ARDS), which causes fluid to leak into the lungs,
2. pneumonia, which inflames the alveoli (air sacs in the lungs) through pus, and
3. multiple organ failure.
Graham Readfearn, a reporter for Full Story, adds that COVID-19 pneumonia has major differences from common pneumonia (Guardian, 2020). The first difference is that COVID-19 pneumonia is viral, which means that medicine alone could not eradicate the virus causing the lung inflammation. For instance, other factors such as temperature and ventilation have to be considered in the treatment. This is contrary to the bacterial nature of common pneumonia, where antibiotics are usually given to treat it.
Furthermore, unlike common pneumonia which mainly swells the alveoli, COVID-19 pneumonia tends to affect not just the air sacs of the lung(s), but the whole lung(s) itself/themselves. As attested by Kotsimbos, “Breathing in and breathing out becomes a challenge.”
A report from McKeever (2020) finds out that COVID-19 could also affect organs outside the respiratory system. They are the following: the digestive system which aids in breaking down the food we eat, the immune system that fights infection inside our body, and the excretory system that expels waste from our body.
First, diarrhea occurs in the digestive system. This is because the virus SARS-CoV-2 could bind with random receptors (protein structures that receive signals and stimulate bodily responses) that match it (Rothan & Byrareddy, 2020). In this case, the virus finds the receptors of the digestive system (i.e. stomach and small intestine) compatible. The process is analogous to fitting a lock (receptor) and key (virus) together.
Second, a surge of cytokines happen in the immune system. At a healthy amount, these proteins signal immune cells to kill harmful bacteria. However, in the case of COVID-19 where multiple tissues are infected, cytokines seem to kill healthy bacteria as well. They cause the extreme complications mentioned above (WHO, 2020).
Lastly, COVID-19 could affect the liver and kidneys of the excretory system, albeit not yet fully investigated. For the former organ, it is important that it has vessels not only carry & filter blood but also secrete enzymes that facilitate body processes. However, these enzymes proliferate in COVID-19, which could lead to the failure of the organ itself (WHO, 2020). On the other hand, the latter organs help in filtering blood through nephrons. However, the nephrons can be injured as small tubes called tubules (in the nephrons) trap the virus.
WHO (2020) states that currently, eight percent of the patients recover, while about 17 percent of them seriously ill. Six percent of the sick get the life-threatening pneumonia and subsequently perish.
Below is a table summarizing the important facts of COVID-19:
Official Names
| Disease: Coronavirus disease (COVID-19) |
| Pathogen: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) | |
Transmission
| Originally, from animals to humans |
| Human-to-human: respiratory droplets (5-10 micrometers), fomites | |
Factors
| Age, having underlying diseases; variable environment conditions |
Effects
| Respiratory system: coughs & colds, shortness of breath, ARDS, pneumonia |
| Others: diarrhea, cytokine storm, nephron injury |
Here is the link for the second part of the scientific guide: http://upismc.blogspot.com/2020/04/health-sciences-consolidated-scientific_8.html.
Sources (in APA format)
• Antrim, A. (2020, March 20). Environmental engineers identify factors affecting COVID-19 transmission. Contemporary Clinic. Retrieved 5 April 2020 from https://contemporaryclinic.pharmacytimes.com/news-views/environmental-engineers-identify-factors-affecting-covid-19-transmission
• Bangkok Post. (2020, January 23). Why wild animals are a key ingredient in China's coronavirus outbreak. Retrieved 4 April 2020 from https://www.bangkokpost.com/world/1842104/why-wild-animals-are-a-key-ingredient-in-chinas-coronavirus-outbreak.
• Centers for Disease Control and Prevention [CDC]. (2020, February 15). Human coronavirus types. Retrieved 2 April 2020 from https://www.cdc.gov/coronavirus/types.html.
• CDC. (2020, April 2). People who are at higher risk for severe illness. Retrieved 5 April 2020 from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html.
• Ducharme, J. (2020, March 11). World Health Organization declares COVID-19 a 'pandemic.' Here's what that means. Time. Retrieved 3 April 2020 from https://time.com/5791661/who-coronavirus-pandemic-declaration/.
• Guardian. (2020, March 18). Coronavirus: the science of how Covid-19 affects the human body. Retrieved 4 April 2020 from https://www.theguardian.com/australia-news/audio/2020/mar/19/coronavirus-the-science-of-how-covid-19-effects-the-human-body?fbclid=IwAR1wZET59EdV0CN0VXjgAVEcIlIodqmk7uO67pfRVS3rIyVRJ0ap_2bW1V4.
• Gutiérrez, P. (2020, April 4). Coronavirus world map: which countries have the most cases and deaths?. Guardian. Retrieved 5 April 2020 from https://www.theguardian.com/world/2020/apr/04/coronavirus-world-map-which-countries-have-the-most-cases-and-deaths.
• Kandola, A. (2020, March 25). How does coronavirus affect the body?. Medical News Today. Retrieved 3 April 2020 from https://www.medicalnewstoday.com/articles/coronavirus-effects-on-body?fbclid=IwAR1CXuLBkO2IyBLksdAj-bSeiq3Ls_DOmCme_QdIidKPz5YU9CqPF1GvlzM.
• McKeever, A. (2020, February 18). Here’s what coronavirus does to the body. National Geographic. Retrieved 3 April 2020 from https://www.nationalgeographic.com/science/2020/02/here-is-what-coronavirus-does-to-the-body/?fbclid=IwAR1cpKImt_PqizPjhGARR2vD4yV3mOjNEsU7QtosFXSWTqGZo0Re_j6rz4g.
• National Institute of Allergy and Infectious Diseases [NAIAD]. (2020, March 25). Coronaviruses. Retrieved 4 April 2020 from https://www.niaid.nih.gov/diseases-conditions/coronaviruses.
• Rothan, H.A. & Byrareddy, S.N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. Retrieved from https://www.sciencedirect.com/science/article/pii/S0896841120300469?via%3Dihub.
• University of California - Los Angeles [UCLA]. (2020, March 20). Study reveals how long COVID-19 remains infectious on cardboard, metal and plastic: People may acquire coronavirus through air and by touching contaminated surfaces. ScienceDaily. Retrieved April 4, 2020 from www.sciencedaily.com/releases/2020/03/200320192755.htm.
• Van Doremalen et al. (2020, March 17). Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. Retrieved 4 April 2020 from https://www.sciencedirect.com/science/article/pii/S0896841120300469?via%3Dihub.
• World Health Organization [WHO]. (2020, February 28). Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Retrieved 4 April 2020 from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
• WHO. (2020, March 18). Basic protective measures against coronavirus. Retrieved 2 April 2020 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
• WHO. (2020, March 29). Vías de transmisión del virus de la COVID-19: repercusiones para las recomendaciones relativas a las precauciones en materia de prevención y control de las infecciones [Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations]. Retrieved 3 April 2020 from https://www.who.int/es/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations.
• Woodward, A. (2020, April 3). It's estimated 1 in 4 coronavirus carriers could be asymptomatic. Here's what we know. Science Daily. Retrieved 4 April 2020 from https://www.sciencealert.com/here-s-what-we-know-so-far-about-those-who-can-pass-corona-without-symptoms.
//by Angelia Albao and James Tolosa
COVID-19,COVID-19 Campaign: How to Identify Valid COVID-19 News
COVID-19 Campaign: How to Identify Valid COVID-19 News
4/07/2020 08:15:00 PM
Media Center
0 Comments
4/07/2020 08:15:00 PM Media Center 0 Comments
COVID-19,COVID-19 Campaign: Paano makakatulong sa panahon ng COVID-19 pandemic?
COVID-19 Campaign: Paano makakatulong sa panahon ng COVID-19 pandemic?
4/06/2020 07:20:00 PM
Media Center
0 Comments
4/06/2020 07:20:00 PM Media Center 0 Comments
COVID-19,COVID-19 Campaign: Mga Karapatan Mo Ngayong ECQ
COVID-19 Campaign: Mga Karapatan Mo Ngayong ECQ
4/06/2020 07:10:00 PM
Media Center
0 Comments
4/06/2020 07:10:00 PM Media Center 0 Comments
Subscribe to:
Posts (Atom)
Welcome
Welcome to Ang Aninag Online!
This is the official blogsite of the UPIS Media Center. Check in every now and then to be updated with the latest UPIS news.
Look into the literary compositions and go through the creative works of various students.
Enjoy and don't forget to leave a comment.
This is the official blogsite of the UPIS Media Center. Check in every now and then to be updated with the latest UPIS news.
Look into the literary compositions and go through the creative works of various students.
Enjoy and don't forget to leave a comment.
Featured Post
Blog Archive
-
▼
2020
(
339
)
-
▼
April
(
16
)
- COVID-19 Campaign: Ano Ambag Nila?
- Pilipinas, tuloy ang laban kontra COVID-19
- COVID-19 Campaign: Hear Their Voices
- COVID-19 Campaign: What Can We Give Our Frontliners?
- Opinion: A vital role on the COVID-19 pandemic
- COVID-19 Campaign: What is the Philippines Doing i...
- COVID-19 Campaign: Countries' Fight against COVID-19
- Health & Sciences: A consolidated scientific guide...
- Health & Sciences: A consolidated scientific guide...
- COVID-19 Campaign: How to Identify Valid COVID-19 ...
- COVID-19 Campaign: #UnaAngMahalaga
- COVID-19 Campaign: #DapatKongkreto
- COVID-19 Campaign: Paano makakatulong sa panahon n...
- COVID-19 Campaign: Mga Karapatan Mo Ngayong ECQ
- COVID-19 Campaign: #DapatTransparent
- COVID-19 Campaign: #NoToVIPTesting
-
▼
April
(
16
)



























0 comments: